The primary results from the RIVER Trial—Rivaroxaban for Valvular Heart disease and Atrial Fibrillation—show that rivaroxaban is comparable to warfarin for patients with bioprosthetic mitral valves. The findings were presented during a late-breaking trial session at the American Heart Association’s Scientific Sessions 2020 (AHA 2020, 13–17 November, virtual).
Researchers say clinicians have used direct oral anticoagulants (DOACs) such as rivaroxaban off-label for patients with bioprosthetic mitral valves who have atrial fibrillation or flutter.
The RIVER trial followed 1,005 patients from 49 sites in Brazil who had a bioprosthetic mitral valve and atrial fibrillation or flutter for 12 months. Patients were randomised to rivaroxaban 20mg once daily or the vitamin K antagonist anticoagulant warfarin (dose-adjusted to an international normalized ratio (INR) between 2.0-3.0). The primary endpoint was a composite of death, major cardiovascular events (stroke, transient ischaemic attack, systemic embolism, valve thrombosis or hospitalization for heart failure) or major bleeding over 12 months.
“This is the largest trial designed to evaluate the safety and efficacy of direct oral anticoagulants in patients with bioprosthetic mitral valves and atrial fibrillation or flutter. Earlier trials of direct oral anticoagulants versus warfarin for atrial fibrillation or flutter together included fewer than 200 patients with bioprosthetic mitral valves,” said lead study author Otavio Berwanger, a cardiologist and epidemiologist, and the director of the Research Institute Hcor, Heart Hospital (Hospital de Coracao) in Sao Paulo, Brazil.
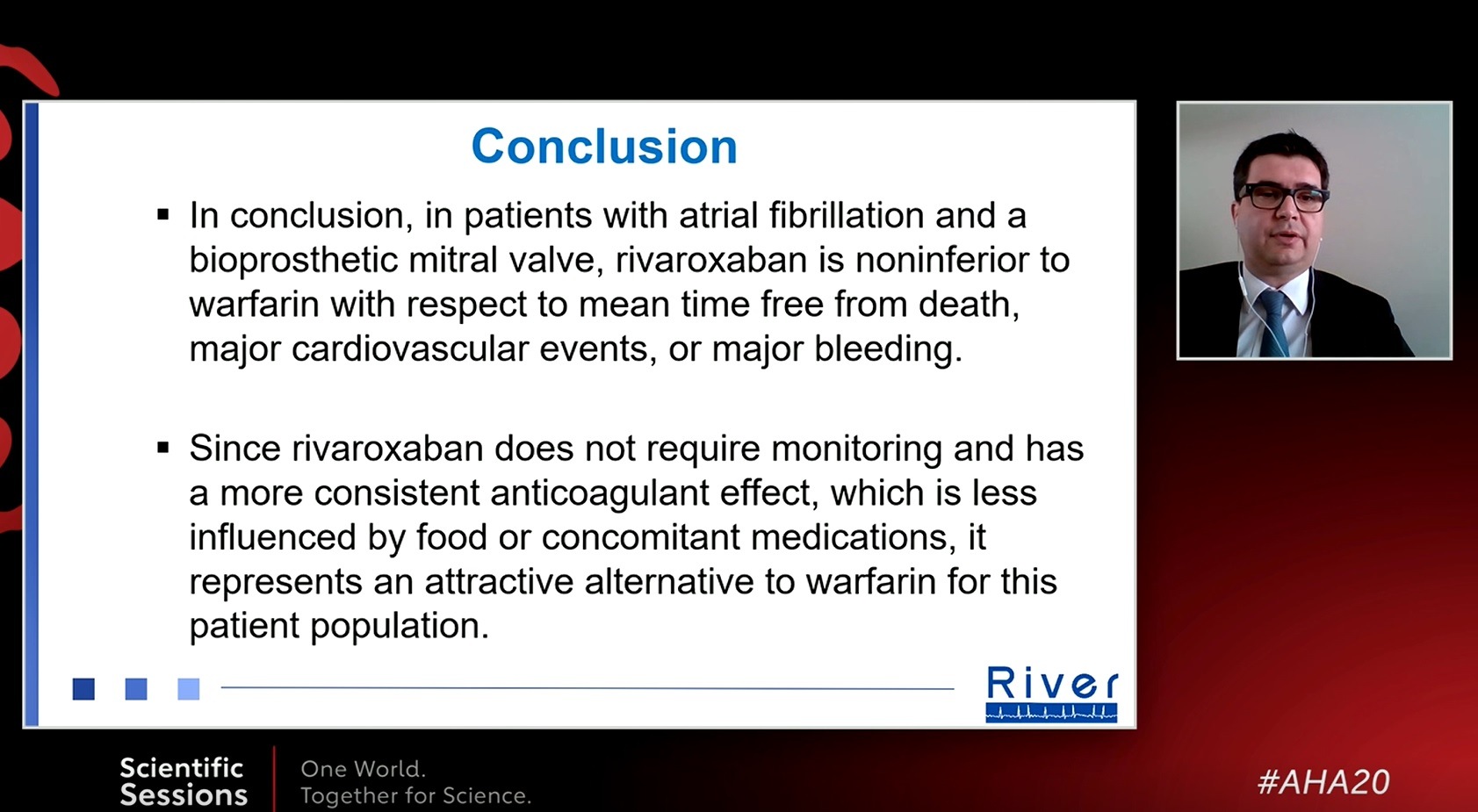
Patients who received rivaroxaban had an average of almost one year (347.5 days) free from the primary endpoint, similar to those treated with warfarin (340.1 days).
“Additionally, our confidence interval likely excluded an effect size larger than 1.4 days free from events favouring warfarin, clearly demonstrating the non-inferiority effect of rivaroxaban in this clinical setting,” Berwanger said. “There was a similarly non-significant numeric trend favouring rivaroxaban for most secondary endpoints, however, the incidence of stroke was lower in the rivaroxaban than in the warfarin group. Importantly, safety events such as valve thrombosis, major/non-major clinically relevant and total bleeding were not statistically different between the rivaroxaban and warfarin groups.”
A subgroup analysis of 18.8% of RIVER patients with bioprosthetic mitral valve implantation within the prior three months showed a mean of 35.1 days longer without evidence of the primary outcome compared to patients treated with warfarin.
“The results from the RIVER Trial are consistent with previous research, including ROCKET and other pivotal trials of DOACs, and can inform clinical practice for patients with bioprosthetic mitral valves,” Berwanger said. “For a subgroup of patients with a mitral valve replacement within the last three months, rivaroxaban was statistically and clinically superior to warfarin.”
The main study limitations are the open-label design, and the fact that the findings cannot be extrapolated to patients with a bioprosthetic aortic valve in the aortic position, or for patients with mitral stenosis or with mechanical valves. Trials in these populations are ongoing.











