This article has been sponsored by Boston Scientific.
Case description
A 62-year-old woman, with recent sinus venosus atrial septal defect correction surgery, developed a persistent macroreentrant atrial tachycardia and macroreentrant atrial tachycardia (MAT) ablation was performed. The diagnosis of this congenital heart defect was done in a cardiac magnetic resonance imaging scanner, performed after an uneventful percutaneous atrial fibrillation ablation carried out in another centre. The patient underwent open-heart sinus venosus defect closure. Early after cardiac surgery, the patient developed an atrial tachycardia and an ablation procedure was scheduled.
A 24-pole catheter (ORBITER®; Bard Medical) was placed around the tricuspid annulus with its distal part within the coronary sinus. Post-pacing intervals at the coronary sinus and right atrium were consistent with right atrial origin of the tachycardia. Right atrial high-resolution activation map performed with the INTELLAMAP ORIONTM 64-poles catheter and RHYTHMIATM navigation system (Boston Scientific, Inc.) showed a macroreentrant circuit with a figure-of-eight involving a broad slow conduction area in the lateral wall of the right atrium (Figure 1): clockwise rotation around the superior vena cava, and counter-clockwise rotation around the inferior vena cava.
The area of slow conduction was located between the two pericaval scars performed at cardiac surgery for extracorporeal circulation, showing phrenic nerve capture along the majority of the line (Figure 2).
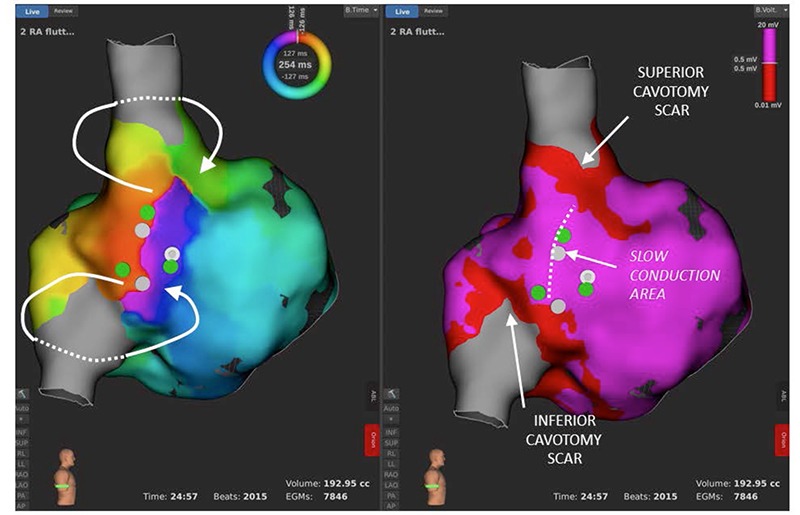
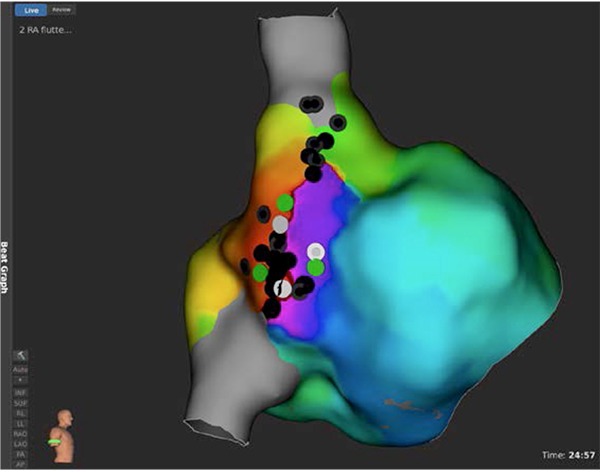
Linear ablation between the two cavotomy scars would have been sufficient to terminate the tachycardia, but that would have implied a high risk of phrenic nerve injury. Hence, high-resolution mapping of this area (previously located with the INTELLAMAP ORIONTM catheter), was done using IntellaTip MIFITM open-irrigated ablation catheter (Boston Scientific, Inc.) in order to localise the critical isthmus of the tachycardia and attempt focal ablation. Spots with the most fragmented signals within the area of slow conduction in the distal dipole of the IntellaTip MIFITM catheter (i.e. potential targets for ablation) were marked in the electroanatomical map (white spots in Figure 1); concealed entrainment with post-pacing intervals that matched tachycardia cycle length was observed from all three locations (green spots in Figure 1).
Mini-electrode signals from these three spots permitted exclusion of false isthmuses (i.e. fragmented electrograms in the distal dipole of the ablation catheter and no fragmented signals in the mini-electrode dipoles, meaning fragmentation at the distal dipole was near-field but not local signal) and selection of the true critical isthmus of the tachycardia (i.e. fragmented electrograms in both the distal dipole of the ablation catheter and the mini-electrode dipoles, meaning local fragmentation at the tip of the ablation catheter). A single application at the most fragmented MiFi electrograms, between the phrenic nerve spots, terminated the tachycardia.
Summary
IntellaTip MIFITM open-irrigated ablation catheter has three mini-electrodes within the distal electrode that allows visualisation of the local electrograms at the catheter tip whilst avoiding near-field signals, which sometimes cannot be distinguished using only the conventional distal dipole signal. Concretely, in the field of MAT, precise location of slow conduction spots is of paramount importance as critical isthmuses that perpetuate the tachycardia usually display slow conduction, represented by fragmented electrograms.
High-density mapping with INTELLAMAP ORIONTM 64-pole catheter and RHYTHMIATM system permits precise documentation of reentrant circuits. Mini-electrodes embedded within the IntellaTip MIFITM open-irrigated ablation catheter allow distinguishing between local, near-field and far-field signals. This may help to select the target for focal ablation in complex tachyarrhythmias.
By Eduardo Franco, Daniel Rodríguez Muñoz, and Javier Moreno, University Hospital Ramón y Cajal (Madrid, Spain)












