 Exposure to bridging therapy independently predicts haemorrhagic complications—without improving functional outcomes—in patients with atrial fibrillation (AF) associated stroke. The findings from this retrospective, registry analysis were presented by Feras Akbik (Emory University, Georgia, USA) during a late-breaking abstract session at the Society of NeuroInterventional Surgery’s (SNIS) annual meeting (4–7 August; virtual event).
Exposure to bridging therapy independently predicts haemorrhagic complications—without improving functional outcomes—in patients with atrial fibrillation (AF) associated stroke. The findings from this retrospective, registry analysis were presented by Feras Akbik (Emory University, Georgia, USA) during a late-breaking abstract session at the Society of NeuroInterventional Surgery’s (SNIS) annual meeting (4–7 August; virtual event).
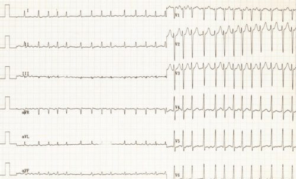
Addressing the online audience, Akbik discussed the rationale behind his research: “Atrial fibrillation is a common and particularly morbid stroke aetiology. In the pre-thrombolysis era, these strokes were associated with larger territories of hypoperfusion and infarction, worse functional outcomes and increased mortality. Even in the thrombolytic era, these patients had increased rates of symptomatic intracranial haemorrhage after IV tPA [tissue plasminogen activator], and still had larger territories of infarction, and, interestingly enough, were less likely to recanalise than other stroke mechanisms.”
Given this, he posed the question: “In the setting of the endovascular era, the question remains: what is the role for IV tPA in these patients?”
The concerns, he said, are “relatively similar” for any other stroke aetiology. “There is thought to be a limited benefit of IV tPA in the setting of large vessel occlusion. There is obviously the concern about IV tPA associated haemorrhage after recanalisation. This is particularly notable given the high rates of recanalisation at most thrombectomy capable centres.”
Akbik also acknowledged that there is also the issue of taking a proximal clot, “thrombolysing” it; pushing it further, and “making what was previously a retrievable clot, now irretrievable”. He argued that the neurointervention field is yet to acquire these answers until randomised data is produced.
Speaking on the datasets available thus far, he said: “SKIP was inconclusive, but DIRECT MT, which was published just a few months back, showed non-inferiority in a relatively small Chinese cohort. There are ongoing trials, MR CLEAN NO IV and SWIFT DIRECT.
However, Akbik told the SNIS audience that by taking a step back, regarding how practice will change, “we have to keep in mind that IV tPA has been the cornerstone for the last 20 years until certain trials came out in 2015.” He argued that it is going to take “a lot” for people to move away from this, and added: “It may not be enough to show non-inferiority or any kind of equivocal data; it may be more important to ask: who gets harmed by bridging therapy?
“The reality is,” Akbik asserted, “these are the AF patients. So the question remains: does bridging therapy have a differential outcome in these patients? Are they less likely to benefit, or more likely to get harmed?”
In order to answer these questions, Akbik said his team leveraged the Stroke thrombectomy and aneurysm (STAR) registry. STAR is an international thrombectomy registry across four continents with over 40 sites included. At the time of this analysis, the team had 4,169 anterior circulation mechanical thrombectomies over a three-year period (2015–2018); a third of which—according to Akbik—had AF, and a third of which had exposure to bridging therapy.
The team first dichotomised the data by AF versus non-AF. “The former are a little older, more likely to be female, and have more vascular risk factors, which is consistent with the general AF stroke literature,” noted Akbik. Looking at their presentation, he said AF patients a more likely to have a higher stroke scale score, a lower Alberta Stroke Program CT Score (ASPECTS), and are less likely to get IV tPA. “But angiographically,” he said, “they have similar outcomes. They have equivalent reperfusion, and equivalent complication rates including haemorrhage.”
In contrast to this, Akbik stated that when looking at bridging therapy patients, “it is a different story”. He said that the team observed so difference in this cohort (mechanical thrombectomy versus mechanical thrombectomy plus IV tPA). However, when examining AF patients exposed to bridging therapy, he said there is a significant increase in haemorrhagic complications, with the absolute risk difference over 2%.
“Now, the question is, what about the confounding variables such as time to presentation? We controlled for this under multivariate assumptions, as well as age and other variables. Even in this analysis we found that IV tPA is the only variable that stands out as a predictor with an Odds Ratio of around two,” Akbik said.
Pivoting to functional outcomes, he claimed there also appears to be a difference. Regarding the shift analysis in the modified Rankin Scale (mRS) curve, Akbik told the audience that there was a “shift in the positive direction” with the mRS in non-AF patients exposed to bridging therapy. Despite this, he noted that when looking at the AF patients, no shift, or benefit, was observed. “There does not appear to be any bang for our buck in terms of bridging therapy in these patients,” he added.
When the team dichotomised the functional outcomes (good versus bad) via multivariate analysis, they witnessed a similar benefit in the non-AF cohort, but again, no benefit signal in AF patients.
Lastly, Akbik alluded to certain caveats of the study. “One is the inherent retrospective biases that come with a registry analysis; two is the mechanisms—it is a comorbid AF versus a TOAST aetiology—so this makes it harder to suss out in a big registry dataset like this. Thirdly, the angiographic and haemorrhagic outcomes are all locally (not centrally) adjudicated. Finally, there is a lack of antithrombotic data in the registry at present.”
He added: “I would point out that the AF patients on anticoagulants, where you worry about bleeding, are those who are least likely to get bridging therapy.”
Despite the limitations, Akbik argued that the current findings highlight the need for randomised trials to assess this high-risk subgroup that may benefit from a more direct thrombectomy approach.
For more stories from SNIS 2020, click here.









