Carlos Morillo (Calgary, Canada) was one of the first physicians to document the potential of ablation of the pulmonary vein region as a strategy to treat atrial fibrillation (AF) experimentally. Born in Bogotá, Colombia, Morillo is currently focusing on the development and implementation of clinical networks that will lead to the necessary infrastructure to conduct clinical trials of neglected diseases such as Chagas and Rheumatic Heart Disease. He has also developed clinical pathways to improve management and assessment of patients with AF and syncope that present to the emergency department. Morillo is a member of the steering committee of many landmark clinical trials including INTERHEART, ORIGIN, CURRENT, OASIS, BENEFIT, ACTIVE, RAAFT, STOP-CHAGAS and POST and has participated as an investigator and a member of the adjudications committees of trials such as ORIGIN, RELY, BENEFIT, AVERROES, RAAFT-2, SIMPLE, amongst others. He talks to Cardiac Rhythm News about the influences on his career, his contributions to the field, and outlines his views on the challenges still to be faced.
When did you decide you wanted a career in medicine?
I think my decision was probably made quite early in life. I come from a family of physicians—my grandfather, my father, two of my brothers, and several uncles and cousins are doctors. Perhaps I had no choice.
My father was a neurophysiologist, and did a lot experimental physiology research. He used to bring me along to his lab at the National Institutes of Health (NIH) in Bethesda, where he worked with several physiology and medicine Nobel prize winners. I would have been about four years old. I have been told I was very inquisitive. I remember going to Tasaki’s lab; he kept a giant squid in an aquarium under his desk. He was among the first to describe synaptic conduction, based on experiments conducted by recording action potentials in the giant squid’s neurons. I was impressed by this.
When we moved back to Colombia, my father conducted experiments where he stimulated areas of the hypothalamus in cats, and could either induce rage or uncontrollable eating. Imagine what it was like for a 10-year-old to go to a lab, and to not only see these experiments, but also to conduct some of your own.
The final push towards a career in medicine came when I was in ninth grade. I had become a bit of a rebel without a cause, and flunked a year. This was unheard of for anyone in my family, so my “punishment” was to work as a lab assistant during the entire summer, under the supervision of a research fellow who was training with my father. We were conducting experiments related to the reticular formation of the brain, described by Magoun and Moruzzi. My father had some theories about the way the reticular formation was activated. My job was to prepare the entire experiment. That consisted of anaesthetising the rabbit, and then performing a tracheotomy. After that, I had to set the rabbit onto a stereotactic device, do a C1‒C2 laminectomy, find the femoral or sural nerve, put some electrodes onto the cortex of the brain, and spend 12 hours stimulating the brain—quite a task for a 13-year-old. At the end of each day, the research fellow and I brought all the recordings to my father who would be sitting on the other side of a huge, intimidating desk. He was a man of few words. He would go through the entire recording, which was a huge stack of paper, barely glimpsing at us over his very thick glasses, and without uttering a word. The outcome was usually the same. He would look at us and say: “Better luck tomorrow. There is nothing here.” He would then toss 12 hours’ work into the bin. I had two options: either I loved it or hated it. I chose the former.
Why did you choose to specialise in cardiac electrophysiology (EP)?
My decision to choose EP was also by chance. I never really felt that I wanted to be a clinician, but rather a scientist. I had applied for a Fogarty International scholarship to go to Stanford University to do a PhD in neurochemistry. I wanted to figure out the physiology of behaviour. I did not get the scholarship, and the chair of Medicine approached me and told me I would be a good clinician. So I did internal medicine, and then cardiology. While I was doing my residency, it became clear to me that the field of EP was where I wanted to go. I came home one evening and my father had left Zipes and Jalife’s first book “From bench to bedside” on my pillow. I read the entire book in a week. The rest is history.
Who were your mentors and what influence did they have on your career?
My first mentor, and the foremost, was my father. He was very influential on my career, always pushing me to be better and more analytical. He gave me both the inspiration and the strength I needed to pursue an academic career—from basic science to evidence-based medicine. In Colombia, my chief of Medicine, Dr Dario Maldonado, was always very supportive, and an outstanding and inspirational clinician. My first chief of Cardiology was Dr Horacio Orejarena at the Military Hospital in Bogotá. He had trained with Forrester, Diamond, Swan, and Ganz, and was incredibly supportive and an astute clinician. Another influence was Orlando Corzo, the head of Interventional Cardiology. He had trained with Andreas Grundzig, and Luis Moya. And, Enrique Melgarejo, who had trained with Agustin Castellanos in Miami as an arrhythmologist, was one of my strongest mentors. We spent hours discussing parasystole, and other arrhythmia mechanisms. They were all very supportive of my inclination to do research, a rare trait in those days in Colombia. Alvaro Mesa, who trained with Al Waldo, was the final encouragement that convinced me to lean towards EP as a lifelong career.
Once I migrated to Canada my most influential mentor was George J Klein. George is a giant in EP, and has made many significant contributions. His uncanny way of teaching and his unreserved support really made a difference to my career. Doug Jones was also instrumental in my formative days. My years at the University of Western Ontario are unforgettable. The AF model we described then has resisted the test of time and continues to be one of my greatest contributions. Ken Ellenbogen and Dwain Eckberg were also very influential during my career as an EP and an autonomic physiologist. Lastly, Stuart Connolly and Salim Yusuf mentored me in the later stages of my career as a clinical trialist, and continue to be very supportive.
You were amongst the first physicians to document the potential of ablation of the pulmonary vein region as a strategy to treat AF experimentally; could you give us more details of this important contribution?
 The University of Western Ontario group pioneered this area and I was part of that group at that time. As an EP fellow in the early 1990s the programme at Western included a mandatory year of experimental EP. I was given the task by George Klein to develop an AF model that did not lead to heart failure. George’s view was that if the atrium was beating fast enough sooner or later AF would develop. His point was that not infrequently patients with atrioventricular nodal re-entrant tachycardia (AVNRT) or atrioventricular reciprocating tachycardia (AVRT) that had regular fast supraventricular tachycardia (SVT) would degenerate into AF. The first challenge was to get a pacemaker capable of being programmed at more than 400ppm. This took some serious negotiating with one of the companies that finally enabled us to have pacemakers pace in the atrium at 400‒600ppm. The first few experiments were a huge failure, after placing the lead in the right atrial appendage and pacing at 400‒600ppm I would check on the dogs the next day, and to my dismay I would find them dead. Autopsy revealed that the atrial lead had migrated to the ventricle and at a pacing rate of 600ppm this led to ventricular tachycardia/ventricular fibrillation (VT/VF)! I learned my lesson fast mostly because I was threatened by George and Doug Jones that I would have to pay for the dogs! This was something I could not afford with a fellow’s salary. I then became a fan of active fixation leads. I had to do weekly echocardiograms to make sure we were not inducing heart failure—we were doing enough structural remodelling such as left and right atrial enlargement but no heart failure. After four to six weeks, I would bring the dogs back to the lab and try to induce AF that was quite easy and sustained for hours. This was not the case prior to pacing at the baseline EP study. As with most discoveries in science, serendipity, boredom and luck come into play and breakthroughs occur. After hours of observing AF I decided to open the chest and do some basic epicardial mapping of both atria. It became quite clear that the left AF cycle length was always faster than the right atrium. Furthermore, consistently this was located to the posterior left atrium around the pulmonary veins. Honestly, I never said the pulmonary veins were the trigger of the rapid atrial pacing AF model. The credit for identifying the pulmonary veins as triggers for AF was put forward by Michel Haïssaguerre and Pierre Jaïs. At any rate again boredom came to play and—given the fact that consistently the AFCL was shorter in the posterior wall around the pulmonary veins—I decided to cryoablate these areas and to my surprise, after a few lesions, AF organised into an atrial flutter and then broke into sinus rhythm. After doing the cryoablation, AF was rendered non-inducible in the majority of the dogs. I remember showing these results to George Klein. He was initially very sceptical, bear in mind this was 1992 and promoting a “focal” mechanism of AF was a blasphemy! I am quite stubborn, so I decided to conduct 20 or 30 experiments more. By then, I had already transitioned into my clinical EP fellowship so I had to conduct the experiments at midnight! After collecting a series of experiments that all showed the same behaviour, I dropped the traces in George’s office. Finally I got his attention. He warned me not to share these results with anyone. I presented this abstract at an American Heart Association (AHA) meeting in 1992 and was given a really hard time for suggesting a “focal” mechanism and worse for suggesting that cryoablating this area “cured” AF. It took me a couple of years to convince the editors of Circulation to publish this paper that actually showed evidence of structural, ultrastructural, and electrical remodelling in addition with identification of an area that was directly linked with the maintenance of AF. All that in a single paper that has over 1,000 citations. Of course, I am biased as I was very involved and committed to get this model published. I learned several lessons, including the fact that a good title makes a difference. Remember: AF begets AF! You cannot beat that!
The University of Western Ontario group pioneered this area and I was part of that group at that time. As an EP fellow in the early 1990s the programme at Western included a mandatory year of experimental EP. I was given the task by George Klein to develop an AF model that did not lead to heart failure. George’s view was that if the atrium was beating fast enough sooner or later AF would develop. His point was that not infrequently patients with atrioventricular nodal re-entrant tachycardia (AVNRT) or atrioventricular reciprocating tachycardia (AVRT) that had regular fast supraventricular tachycardia (SVT) would degenerate into AF. The first challenge was to get a pacemaker capable of being programmed at more than 400ppm. This took some serious negotiating with one of the companies that finally enabled us to have pacemakers pace in the atrium at 400‒600ppm. The first few experiments were a huge failure, after placing the lead in the right atrial appendage and pacing at 400‒600ppm I would check on the dogs the next day, and to my dismay I would find them dead. Autopsy revealed that the atrial lead had migrated to the ventricle and at a pacing rate of 600ppm this led to ventricular tachycardia/ventricular fibrillation (VT/VF)! I learned my lesson fast mostly because I was threatened by George and Doug Jones that I would have to pay for the dogs! This was something I could not afford with a fellow’s salary. I then became a fan of active fixation leads. I had to do weekly echocardiograms to make sure we were not inducing heart failure—we were doing enough structural remodelling such as left and right atrial enlargement but no heart failure. After four to six weeks, I would bring the dogs back to the lab and try to induce AF that was quite easy and sustained for hours. This was not the case prior to pacing at the baseline EP study. As with most discoveries in science, serendipity, boredom and luck come into play and breakthroughs occur. After hours of observing AF I decided to open the chest and do some basic epicardial mapping of both atria. It became quite clear that the left AF cycle length was always faster than the right atrium. Furthermore, consistently this was located to the posterior left atrium around the pulmonary veins. Honestly, I never said the pulmonary veins were the trigger of the rapid atrial pacing AF model. The credit for identifying the pulmonary veins as triggers for AF was put forward by Michel Haïssaguerre and Pierre Jaïs. At any rate again boredom came to play and—given the fact that consistently the AFCL was shorter in the posterior wall around the pulmonary veins—I decided to cryoablate these areas and to my surprise, after a few lesions, AF organised into an atrial flutter and then broke into sinus rhythm. After doing the cryoablation, AF was rendered non-inducible in the majority of the dogs. I remember showing these results to George Klein. He was initially very sceptical, bear in mind this was 1992 and promoting a “focal” mechanism of AF was a blasphemy! I am quite stubborn, so I decided to conduct 20 or 30 experiments more. By then, I had already transitioned into my clinical EP fellowship so I had to conduct the experiments at midnight! After collecting a series of experiments that all showed the same behaviour, I dropped the traces in George’s office. Finally I got his attention. He warned me not to share these results with anyone. I presented this abstract at an American Heart Association (AHA) meeting in 1992 and was given a really hard time for suggesting a “focal” mechanism and worse for suggesting that cryoablating this area “cured” AF. It took me a couple of years to convince the editors of Circulation to publish this paper that actually showed evidence of structural, ultrastructural, and electrical remodelling in addition with identification of an area that was directly linked with the maintenance of AF. All that in a single paper that has over 1,000 citations. Of course, I am biased as I was very involved and committed to get this model published. I learned several lessons, including the fact that a good title makes a difference. Remember: AF begets AF! You cannot beat that!
In your view, what has been the most important development in cardiac rhythm management during your career?
There have been a lot of major developments. When I started my training, I spent most of the day in the operating room with Gerard Guirardon, performing surgery for Wolff-Parkinson White syndrome. In less than 12 months, catheters that delivered radiofrequency energy became available, and it suddenly changed the entire field. EP is one of the few fields in medicine where we cure patients. I was in London when the first transvenous implantable cardiac device (ICD) was implanted, and the first implantable loop recorder. When we developed the rapid atrial pacing AF model, ablation of AF was considered blasphemy. Another improvement is that we have four new anticoagulants. There has been so much progress made during my career that I could not single out one thing only.
Could you tell us about one of your most memorable clinical cases?
My most memorable case happened during my second year on internal medicine residency. A young woman came to the hospital with acute pulmonary oedema, and the chest X-ray showed pulmonary oedema with a ‘normal’ cardiac silhouette and AF. This was in the 1980s in Colombia when we did not have echo availability in the middle of the night. Getting a history was tough because the patient was a deaf-mute. I did not hear any murmurs when I auscultated her. She was anaemic and had a few other findings, and the chief resident and I made some differential diagnoses, but we felt it was most likely that she had haemosiderosis. The next day, the chief of medicine, Dr Maldonado, came to do his rounds. He looked at the chest X-ray and the ECG, and palpated her chest. Then he looked at me, and said: “This is a classic severe mitral stenosis. Get an echocardiogram stat.” It turned out that it was mitral stenosis, and I had to present this case in grand rounds. The mitral stenosis was so severe that it did not create a murmur. I remember trying to justify my misdiagnosis based on the fact that the lady was a deaf-mute, and therefore she had a ‘mute’ severe mitral stenosis.
What are your current areas of research?
AF mostly in clinical trials determining the best treatment in both paroxysmal and persistent AF. Also, subclinical AF, and its impact on screening and management. Other areas are the detection of AF in cryptogenic stroke, oral anticoagulation in cardioversion and AF ablation, syncope, and Chagas disease.
As a physician with vast research experience in syncope, what are the key unanswered questions in the field?
Despite significant improvements in our diagnosis and management of syncope, we still have gaps in translating this knowledge to family physicians, internists, and cardiologists. We continue to work towards achieving this goal, as well as understanding how to minimise inappropriate testing and hospital admissions in syncope. We are also still searching for the most effective treatment for vasovagal syncope, and for how to choose the ideal patient for implantable cardiac monitors.
In 2015 you published the results of BENEFIT, the largest trial in Chagas disease. After these results, what is the best method of treatment, and how much hope is there of finding a cure?
With the BENEFIT (Benznidazole evaluation for interrupting trypanosomiasis) trial we showed that the treatment regimen used with benznidazole—the care standard—did not influence the progression of Chagas cardiomyopathy. However, we did show, in some regions, significant reduction in parasite detection, although unfortunately that was not persistent. These findings should be interpreted with caution, and do not mean that treatment with trypanocidal drugs is not justified. We need more effective treatments. This could be a combination therapy, and repeated treatment. Furthermore, treatment before the cardiomyopathy stage is manifest should be encouraged. There is always hope of finding a cure.
Could you tell us the positive and negative aspects of developing and implementing clinical networks to conduct clinical trials of neglected diseases such as Chagas disease?
Creating and implementing the infrastructure to conduct clinical trials that are focused on neglected diseases has significantly more positive than negative aspects. Nothing is more positive than the global interest that both the BENEFIT and STOP-CHAGAS (Study of the use of oral Posaconazole [POS] in the treatment of asymptomatic chronic Chagas disease) trials have triggered. One of the main goals was to create international awareness of this neglected disease, which has become global due to migration patterns. We have achieved this goal, and the renewal of interest has attracted the attention of the pharmaceutical industry, which is hoping to develop new molecules and treatments for this devastating disease. We have fostered a sense of pride in all the participating centres, and that can only lead to more, and better, research. We created and built the capacity to establish three high quality PCR core labs, and further developed the technology required to use PCR within the context of a clinical trial. Conducting these trials is challenging. Raising funds and creating the appropriate infrastructure can sometimes be frustrating. But I do not perceive any of these challenges to be negative. They build character.
As a Latin American physician with vast experience working in Colombia and Canada; could you tell us what Canadian physicians could adopt from best practice in Colombia and vice versa?
Gaps in practice and care have markedly changed in both Canada and Colombia compared to when I was in medical school. Nowadays, Colombia is considered a middle-income country, with a two-tiered heathcare system. The main challenge there is access to care. Canadian physicians could learn about the excellent clinical skills achieved in countries like Colombia, because of limited access to technology. Physicians must choose what tests to perform very wisely, based on the limited availability. And Colombian physicians could adopt the more evidence-based medical practices that are well established at all levels of care in Canada.
What do you consider are the biggest challenges with the practice of EP in Latin America?
As I mentioned, access to care and technology is a limitation in most countries in Latin America. Some countries like Mexico have the lowest ICD implant rates in the world. Some of these limitations are related to the cost of technology, and others to knowing how to translate clinical trials into everyday practice. But, Latin America is continuously evolving, and countries like Brazil and Colombia are leading the way in rapid change and the implementation of best practice and the rational use of technology in EP.
If you had not been a medical doctor, what would you have been?
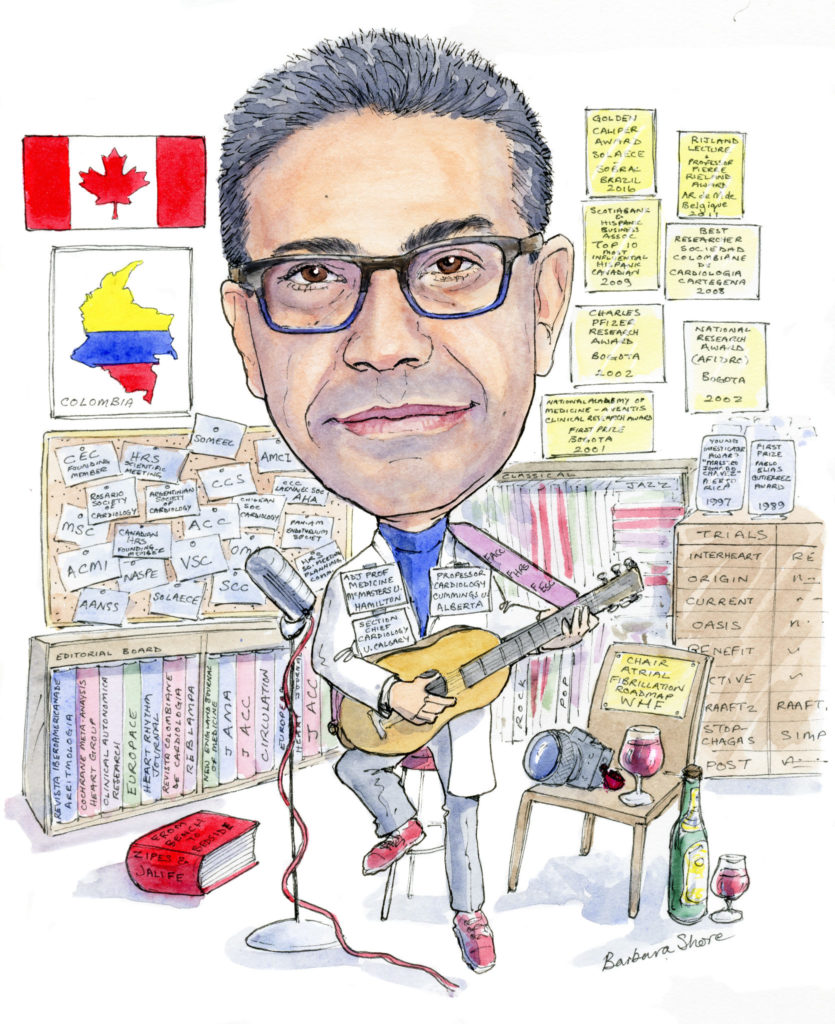
I have some musical inclinations; I like singing and playing the guitar. I am also an acceptable photographer. My father had a darkroom at home, and we all learned how to develop photographs. Not that it matters in this digital era.
Outside of medicine, what other hobbies or interests do you have?
I have a vast collection of music—more than 5,000 CDs, LPs, and cassette tapes. I like all genres, but my favourites are jazz and choral music. I usually look for the jazz clubs in every city I visit and enjoy a good evening of live music. I also like photography and hiking. I am a ‘foodie’, and have been to some of the finest restaurants on the planet—always combined with good wine and some great company.
Fact File
Current principal clinical and hospital responsibilities
2016– Zone Head, Cardiology Calgary & Southeastern Region, Alberta Health Services
2016– Section Chief, Cardiology Division, Libin Cardiovascular Institute, University of Calgary, Staff Cardiologist & Electrophysiologist Foothills Medical Centre
2002– Director, Syncope and Autonomic Dysfunction Unit, Hamilton Health Sciences, Hamilton, Canada
2003– Staff Cardiologist, Cardiac Electrophysiology and Autonomic Disorder Clinic, Hamilton, Health Sciences Corporation, McMaster University, Hamilton, Canada
1996– Chairman, Department of Cardiology and Cardiovascular Sciences, Fundación Cardiovascular del Oriente Colombiano, Universidad Industrial de Santander, Bucaramanga, Colombia
1996– Director, Autonomic Physiology and Cardiac Electrophysiology Laboratory, Fundación Cardiovascular del Oriente Colombiano, Bucaramanga,Colombia
Recent academic appointments
2016– Section Chief, Cardiology Division, Department of Cardiac Sciences, University of Calgary, Libin Cardiovascular Institute, Zone Head Cardiology Calgary and Southeastern Alberta Region, Alberta Health Services
2016– Professor, Department of Cardiac Sciences, Division of Cardiology, Cumming School of Medicine, University of Calgary, Calgary, Canada
2016– Adjunct Full Professor, Department, of Medicine, McMaster University, Associate Scientist, Neglected Diseases and Arrhythmias, Population Health Research Institute HHSC, Hamilton, Canada
Other professional activities (selected)
2016– Chair, World Heart Federation Atrial Fibrillation Global Roadmaps
2016– Member, Editorial Board Heart
2016– Canadian Representative Executive Board, International Cardiovascular Pharmacology Society
2015– Member, Editorial Board HeartRhythm Journal
2013– Heart Rhythm Society ‒ Latin America Ambassador







