A novel cardiac ablation system may hold the potential to improve upon the currently available treatments for ventricular arrhythmia (VA) patients, having demonstrated positive safety signals in a European registry study including more than 100 of these typically challenging cases.
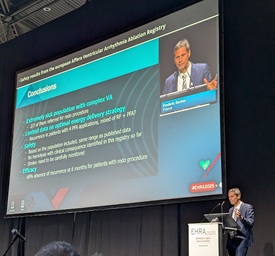
Safety data on this technology—the Affera mapping and ablation system (Medtronic), which offers the potential to treat arrhythmias using both pulsed field ablation (PFA) and radiofrequency (RF) ablation—were shared via a late-breaking presentation from Frédéric Sacher (LIRYC Institute, Bordeaux University Hospital, Bordeaux, France) at the recent European Heart Rhythm Association (EHRA) congress (30 March–1 April 2025, Vienna, Austria).
Sacher originally noted on behalf of his co-authors that, while PFA has emerged as an increasingly popular approach to treating atrial fibrillation (AF) in recent years, the modality also represents a “potentially very interesting” option in VA—with early-stage studies having already hinted at the positive impact it could have for these cases.
With this in mind, investigators for the AVAAR registry sought to evaluate the safety of complex VA ablation cases utilising the Affera device, with a total 126 procedures from 16 European centres being included. Their primary endpoint was the rate of complications during or within 24 hours of the procedure.
Throughout his presentation, Sacher emphasised the fact that the study involved a challenging population of “extremely sick” patients, roughly 80% of whom had non-ischaemic cardiomyopathy (NICM) and two-thirds of whom had been referred for a ‘redo procedure’.
Moving on to outline the study’s safety outcomes, he reported a 6% rate of major acute complications during or within 24 hours of the ablation procedure—including four procedure-related complications and three ‘potentially device-related’ complications. The presenter also relayed a 15% rate of minor acute complications within the same timeframe, which included five procedure-related complications and a total of 14 potentially device-related complications.
Overall, four deaths occurred at the one-month follow-up timepoint in the study, and—in terms of efficacy-related outcomes—the investigators observed a 68% rate of absence from VA recurrence in patients undergoing a redo procedure.
Discussing the implications of these findings from the AVAAR registry, Sacher commented that limited data are available on the optimal energy delivery strategy in this space, and that the benefit of a PFA-only approach versus PFA plus RF ablation “remains to be determined”. He went on to note that the registry’s safety results are comparable to previously published data on similar patient populations, adding that no haemolysis “with clinical consequence” has been identified in their analyses to date, but risks of stroke need to be “carefully monitored and reported” moving forward.
Providing a presentation reviewing these data at EHRA, Gerhard Hindricks (Deutsches Herzzentrum der Charité, Berlin, Germany) stated: “Ladies and gentlemen, PFA has arrived at the ventricles.”
Continuing, Hindricks described this research as an “important step” in the further exploration of the implementation of a new technology for catheter ablation.
“It is particularly important, after the many interesting and important studies we have seen with the application of PFA in the field of atrial fibrillation, that we now—in a very structured manner—move into the field of ventricular tachycardia in patients with structural heart disease,” he added. “Why is this so important? Because, for many, many decades, we have really been struggling with the extreme challenges of improving the outcome of catheter ablation for ventricular tachycardia and ventricular fibrillation in patients with structural heart disease. We have to admit that the recurrence rates are still very high—particularly in patients with ischaemic and non-ischaemic cardiomyopathy.”
Hindricks concluded by noting that these results are “encouraging”, despite their preliminary nature.









