Use of temperature-controlled ablation for the treatment of atrial fibrillation (AF) is effective and highly efficient, according to Jose Osorio—the director of electrophysiology at Grandview Medical Center in Birmingham, Alabama, USA. His comments follow the completion of a US-based clinical trial, evaluating the safety and efficacy of a new ablation catheter, the QDot Micro Catheter (Biosense Webster), which he presented at AF symposium 2022 (13—15 January, New York City, USA) earlier this year. Here he tells Cardiac Rhythm News about the findings of the Q-FFICIENCY trial and recent technological advancements in ablation technology.
Can you give a brief overview of the study background and objectives?
The Q-FFICIENCY trial was a US-based clinical trial, evaluating a new ablation catheter called the QDot Micro. This ablation catheter has a unique design that allows, once again, to conduct ablation with a temperature control mode, which is something we had lost over the years, with irrigated catheter ablation. We had 191 patients enrolled in the trial and followed for one year post-ablation, looking at efficacy and safety.
What was the driving force for this project and what led to the creation of this device?
Over a decade ago, we started using irrigated catheters for most procedures, which allowed us to safely deliver higher power without the fear of char formation. However, that limited our ability to measure the temperature of the tissue catheter interface accurately. So, largely our ablations have been controlled with what we call a ‘power control mode’, which does not use temperature.
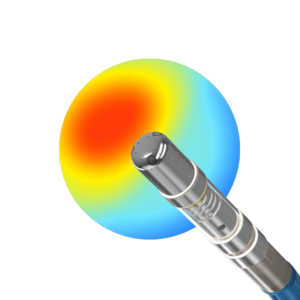
This catheter, the QDot Micro—because of the six-thermocouple design and positioning in the distal part in the tip of the ablation catheter—is now allowing us to carry out ablation using temperature control. On top of that, it has other features that allow the procedure to be done safely.
The driving force was to get us the ability to bring back temperature control ablation. The catheter allows you to use the temperature control mode in two different ways—one that is very high power and short duration—with 90 watts of power. This is higher than we typically use in traditional catheters, known as ‘QMode+ mode’. In this mode, 90 watts are delivered for up to four seconds by the catheter measuring the temperature.
The second mode is called ‘QMode’, with conventional power and temperature control allowing you to do ablation at whatever power you choose. Essentially, what that means is temperature control after the system is measuring the temperature in real-time—if the temperature rises it decreases the power to maintain a safe and effective level of temperature throughout the ablation.
What does the device offer compared to current methods of ablation?
The first advantage of this catheter would be the temperature measurement using six thermocouples. The second is three microelectrodes that allow you to look at high fidelity electrograms within the area you are ablating. The third is the irrigation property of this catheter—it has a porous tip with a different irrigation design than most catheters available today. These three features, together with the fact that QDot Micro is fully integrated into an electro anatomical mapping system, is what make this catheter unique and that is what we tested in the trial. A very high-power short-duration mode, 90 watts, for up to four seconds was the primary mode used in the trial, and the second was the conventional-power temperature-controlled mode, called QMode.
What were the primary findings of the study? Did you find anything surprising?
What we were hoping to see, and what we saw, is that this catheter allowed us to do the ablations in a very efficient way—with procedure times, ablation times, and fluoroscopy times that were rather decreased compared to other studies that were similarly designed, with success rates at one year which were better than other studies, with both improved efficiency and efficacy without compromising safety.
Do you think the use of this device could become more widespread?
I think so, due to the flexibility we have using this catheter, as it allows you to perform ablation using the two modes, the very high-power short duration, and conventional power in a temperature control mode. It makes a really flexible catheter, giving physicians the opportunity to choose what is the right mode of ablation for different areas of the heart, depending on whether you have thick or thinner tissue. This is quite an important feature.
I do expect that this catheter will provide an important toolset for electrophysiologists, particularly during AF ablation which has been tested on this trial, but possibly, even other ablations. The catheter is already approved in Europe and Japan. The US Food and Drug Administration is currently evaluating the data, and US approval is expected later this year.

Do you think the findings of Q-FFICIENCY will have significance for practice?
Absolutely—if you summarize the findings of improved outcomes at 12-months in terms of effectiveness in comparison with previous studies that were similarly designed, we saw better freedom from recurrence of AF at 12 months, which was better than other studies. In this trial, the procedures were faster with a similar safety profile—I think this would be a very welcome addition to the catheters we are able to use today.
Are there any further steps needed in the future of this device?
This study was a large well designed investigational device exemption study, looking at safety and efficacy in terms of what is needed for the approval of the catheter—I do not think there will be other studies needed. There are other studies going on right now in Europe, trying to understand the differences between the QMode+ (90 watts for up to four seconds) and the conventional power with temperature control mode (QMode). There is an ongoing trial randomising patients to one mode versus the other—carrying out AF ablation—to see if one is better than the other. Remember that in the current trial, we are discussing the QMode+, 90 watts ablation as the primary ablation mode. If we were not able to obtain isolation using that mode, we switched to the conventional power with the temperature control mode. As the utilisation of this catheter increases and physicians have gained more experience, there are many physicians only using this very high-power short duration mode and seeing good outcomes, and this enhances the idea of the trial comparing one mode versus the other.
Could you give a summary of the key messages of the Q-FFICIENCY trial?
To me, the importance of this catheter is the ability to bring back temperature-controlled ablation. That allows us to really deliver radiofrequency at very high power, at 90 watts for a very short period. Our hope was to see improved results, and we certainly saw this in this clinical trial. The summary of this trial is that with this new catheter, in comparison with other similarly designed trials, we have seen a faster, safe, and more effective procedure, with success rates at one year with freedom from recurrence of 82% and clinical success (i.e., freedom from symptomatic recurrence) of almost 90%. It is striking that the technological evolution we have had over the past 10 years, getting us clinical success from 70% to almost 90% with this technology, so this is the most important aspect to be highlighted.









