By Angela Gonzalez
Results from the INOVATE-HF trial indicate that vagus nerve stimulation does not reduce the rate of death or heart failure events in chronic heart failure patients. The data were simultaneously presented at ACC 2016 and published in the Journal of the American College of Cardiology.
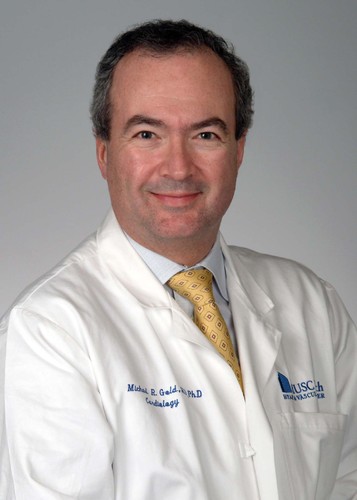
The INOVATE-HF (Increase of vagal tone in chronic heart failure) trial “was the first large, randomised trial of device-based autonomic modulation in heart failure,” write the authors, led by Michael R Gold, Medical University of South Carolina, Charleston, USA. The study was an international, randomised, open-label clinical trial exploring the impact of vagus nerve stimulation on patients with heart failure and a reduced ejection fraction, which is still “the leading cause of hospitalisation in adults in the USA.” Autonomic imbalance, with excess sympathetic activation and decreased vagal tone, is “an integral component of the pathophysiology of heart failure”, and thus has been the target of many new therapies. Of these, vagus nerve stimulation is the “best studied,” note Gold and colleagues.
Pre-clinical studies have demonstrated the benefit of vagus nerve stimulation in reducing mortality, improving cardiac function and decreasing inflammation in a variety of animal models of heart failure. Based on these data, several clinical studies have been carried out, including the six-month NECTAR-HF and ANTHEM-AF trials. The NECTAR-HF trial compared vagus nerve stimulation with medical therapy in 96 patients, finding that the primary endpoint of the trial-the change in left ventricular (LV) end-systolic diameter-did not improve with vagus nerve stimulation, although it did produce a significant increase in quality of life. In the ANTHEM-AF trial, 60 patients were randomised to left- or right-sided vagus nerve stimulation, with both arms of the study showing significantly improved echocardiographic measures of reverse remodelling.
The INOVATE-HF trial involved 85 centres and 707 patients with chronic heart failure, New York Heart Association Class III symptoms and ejection fraction <40%. Patients were assigned to device implantation (CardioFit System; BioControl Medical) to provide vagus nerve stimulation (active group) or continued medical therapy (control group) in a 3:2 ratio. The CardioFit System includes a lead to sense the heartbeat, as well as a lead that sends electrical stimulation to a cuff around the vagus nerve, which is the primary conduit between the parasympathetic nervous system and the heart.
After a one-month healing period, nerve stimulation patients underwent multiple scheduled visits over a four-week period, during which time the stimulation output was gradually increased with a goal of achieving current of 3.5–5.5mA. In the control group, pre-planned study visits were also scheduled so that the number of contacts with the study team could be roughly equivalent to the active group. The primary efficacy endpoint was the composite of death from any cause or first event for worsening heart failure.
Patients were followed for a mean of 16 months (range 0.1–52 months), with a study visit compliance rate among patients of 98%. The primary efficacy outcome occurred in 132 of 436 patients in the vagus nerve stimulation group, compared with 70 of 271 in the control group (30.3% vs. 25.8%; hazard ratio 1.14; 95% confidence interval, 0.86–1.53; p=0.37). During the trial, the estimated annual mortality rates were 9.3% and 7.1% for the vagus nerve stimulation and control groups, respectively (p=0.19). Quality of life, New York Heart Association Class and six-minute walking distance were favourably affected by vagus nerve stimulation (p< 0.05), but left ventricular endsystolic volume index was no different (p=0.49). Despite the secondary benefits, Gold et al write, “The primary results of this study show that vagus nerve stimulation was not effective for reducing the rate of death from any cause or heart failure events. Moreover, vagus nerve stimulation did not promote reverse remodelling in this population.”
The authors continue, suggesting that, “The mixed results from INOVATE-HF and previous vagus nerve simulation studies has also been noted with other device therapies in heart failure such as spinal cord stimulation. This probably illustrates the complexity of autonomic modulation with many different factors that may affect outcomes, including trial design, stimulation parameter (such as site, frequency, and intensity) and the patient population under study.”