Cryoablation showed superior to anti-arrhythmic drug therapy in a study presented during late-breaking sessions at the 59th Annual Scientific Session of the American College of Cardiology in Atlanta, USA.
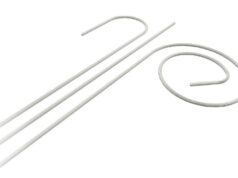
In the STOP AF (Sustained treatment of paroxysmal atrial fibrillation) trial, 69.9% of patients with paroxysmal atrial fibrillation treated with the Arctic Front Cardiac CryoAblation Catheter System (Medtronic) remained free of atrial fibrillation (AF) one year after cryoablation, compared to 7.3% on drug therapy.
All primary safety and effectiveness endpoints in the trial were met.
“These data are a promising indication of the safety profile of cryoablation and its effectiveness in isolating the pulmonary veins to stop AF,” said Kevin Wheelan, chief of staff at Baylor Heart and Vascular in Dallas, USA, and investigator with the STOP AF trial. “The cryoballoon demonstrated strong results in treating paroxysmal AF patients who had previously failed drug treatment.”
As presented by Douglas Packer, professor of Medicine, Mayo Clinic in Rochester, USA, and principal investigator, the STOP AF study randomised patients to receive either cryoablation or anti-arrhythmic drug therapy. For every three patients enrolled, approximately two received an ablation and one was randomly assigned to the drug therapy group. Twenty-six US and Canadian centres enrolled 245 patients (163 cryoablation and 82 anti-arrhythmic drugs). Outcomes on all patients were assessed through 12-months of follow-up. These results are part of the PMA submission in consideration for FDA approval for the Arctic Front Cardiac CryoAblation Catheter System.
The primary effectiveness outcome was treatment success and was defined as having both acute procedural success and freedom from chronic treatment failure for those patients randomised to cryoablation. Acute procedural success was defined as demonstration of electrical isolation in three or more pulmonary veins at the conclusion of the first cryoablation procedure. Using this definition, acute procedural success was achieved in 98.2% (160/163) of cryoablation patients. Chronic treatment failure was defined as the occurrence of detectable AF after a 90-day blanking period (the time after treatment when an AF event is not counted). Chronic treatment failure also included the occurrence of an AF intervention or the use of a non-protocol AF drug anytime during the 12-month follow up. At 12 months, 69.9% of cryoablation patients demonstrated treatment success compared to 7.3% of anti-arrhythmic drug patients.
The two primary safety outcome measures were Cryoablation Procedure Events (CPEs) in cryoablation subjects and major atrial fibrillation events (MAFEs) in both study groups. The data indicate that both primary safety outcomes were met. Cryoablation patients with one or more CPEs was 3.1% with a one-sided 95% upper confidence bound of 6.3%, which was significantly less than the 14.8% pre-specified upper confidence bound (p<0.001). No treatment-related deaths or atrioesophageal fistulas were reported. In addition, 96.9% of cryoablation patients were free from MAFEs, compared to 91.5% of drug patients (p<0.001, non-inferiority).
The trial also captured safety data on several of the more common complications of any ablation procedure in 228 patients that underwent cryoablation procedures including those randomised to cryoablation (163) and those who crossed over for cryoablation (65) after failing drug therapy. Phrenic nerve palsy, a recognised observation with this technology, was noted after 11.2% of all cryoablation procedures (29/259) in 228 patients. At 12 months, 224 of the 228 patients (98.2%) that received a cryoablation were free of any effects related to phrenic nerve injury. In other safety findings, seven patients (3.1%) developed pulmonary vein stenosis; only two required treatment. Across clinical trials there is considerable variation in the definition and calculation of pulmonary vein stenosis. In STOP AF, pulmonary vein stenosis was defined as a reduction in the calculated pulmonary vein cross-sectional area to less than 25% of the baseline pulmonary vein cross-sectional area. A vein that was stenotic at anytime during study follow-up was considered stenotic for this analysis.
The Arctic Front Cardiac CryoAblation Catheter System is commercially available for use in Europe and certain other countries outside the United States and is under investigational use in the United States.